This post is about the risks of controlled crying, because the benefits are pretty straight forward - if it works, your child stops waking you up and you get more sleep. There is no evidence that controlled crying actually results in more sleep for a child, a child with a more independent personality, or a better sleeper in the long run.
WARNING: If you have already done controlled crying with your baby, please be warned that this post may not be something you want to read. It is about the potential downside of the practice. If you have done it and are happy with the result, why stress yourself about might-have-beens? This post is really written for those parents considering whether they will do crying / self-settling. If you have done cc and still want to read this post, then please also read this explanation about how the information should be viewed in context.
This post is the third in a series on sleep. You may want to read Part 1: What is a Normal Sleep? And Part 2: Effectiveness of Controlled Crying.
A big thanks to Giselle Condos for her feedback and advice on writing on this extremely difficult topic - although all mistakes in the end are mine! This is an extremely large and complex topic. If you feel I have misinterpreted or overlooked important information, please leave a comment and bring it to my attention.
The arguments in summary
Those arguing in favour of controlled crying would argue that the method teaches a child to fall asleep without assistance, empowering the child to soothe themselves and be more independent. They would argue that the disruption to a family of a poor sleeper outweighs any detriment caused by the crying itself, and that a child has to learn that they don't always get what they want.
Those arguing against controlled crying would argue that the child does not truly learn to 'self-soothe', but rather learns not to communicate their distress to their parents. They would argue that the early years are a critical time for a child to develop resilience and good mental health, and that the the foundations of pro-social behaviour and resilience is a loving 'attached' relationship with their primary caregiver. They would argue that a young child who has been left to cry feels intensely that they have been abandoned by those they love, and this is not a small discomfort but a terrifying ordeal that they do not have the cognitive skills to rationalise. They would argue that crying methods teach a child that it is normal relationship behaviour to be abandoned by those they love, giving rise to clingier and anti-social attention-seeking behaviour as the child grows older, and a loss of trust and respect towards the parents by the child.
The answer in summary
Very little research has been done on the effects of controlled crying, which means whether it is 'safe' or not is all a bit speculative. However, the following points can be made:
- babies under about 6 months don't really notice if they are separated from their mums, but they are not capable of choosing to calm themselves down when they become stressed, the infant-carer relationship has evolved in such a way that the child expects and relies on an adult to help soothe them - this is healthy and natural, and there is no reason to think 'breaking' this habit assists the child's development generally;
- activities like sucking can genuinely be soothing to a baby and have been shown to reduce stress hormones (Mörelius et al.) - so it is possible that at least some babies genuinely learn techniques to self-soothe,
- just because some babies self-soothe, it does not follow that all babies will stumble onto self-soothing techniques if left to their own devices;
- it is very difficult to know whether a young baby is self-soothing or whether they have learned to passively accept that a state of disorganisation / stress is normal;
- there is no evidence to suggest that babies who sleep through the night from an early age are smarter, more advanced, or more independent (in a general sense) than babies who do not - self-settling shouldn't be confused with learning to be independent in the sense of greater self-esteem or thinking for oneself;
- sometime, usually between 6-9 months, babies develop 'separation anxiety', becoming stressed if they are separated from their primary caregivers (although the stress does not occur if a sensitive substitute caregiver stays with them and meets their needs);
- repeated or intensely stressful experiences during the first two years of life can actually change the way the brain develops;
- if the stress is overwhelming and the child feels so overwhelmed they give up on solving it, the brain becomes hardwired for anxiety, depression, submission, and helplessness;
- if the stress is unpleasant but not overwhelming, the child may cope by reducing their level of sensitivity to stress generally – however this 'switching off' has some unpleasant side-effects, including reducing the child's ability to appreciate their effect on others, and making it harder for the child to remember new information.
- infants and toddlers whose parents are consistent and sensitive in meeting their needs are more likely to have better behaviour, self-esteem, and relationship patterns as they grow older - there is debate over when this formative period ends, some suggesting 6 months, some suggesting 9 months, and some suggesting 18 months;
- some infants are at risk of damage from early childhood stresses - they appear to be born with the kind of 'fearful' and passive personalities (their ‘temperament’) – and failure to be consistent and sensitive to these infants strongly predicts the development of anxiety disorders down the track;
- maternal depression makes it more likely a baby will have an ‘at risk’ temperament; and
- a child who has suffered negative effects from controlled crying would not necessarily 'act out' in ways a parent recognises as negative – rather, a young baby would manifest problems in terms of being generally unmotivated and prone to giving up easily in the face of frustration, whereas a toddler might be anxious to please by 'being good' but become very high strung and show excessive irrational fears.
If controlled crying is not repeated and repeated, if the child is usually caringly and responsively attended to, and if the child still remains capable of healthy expressions of anger, joy and determination, it seems the child may have genuinely learned to self-soothe and it is unlikely than any damage would have been done. On the other hand, if a baby responds to controlled crying by becoming EITHER placid and obedient, OR clingy and anxious (these are two different but maladaptive responses), this should be a big red warning sign to the parents that the child has not learned to self-soothe but rather learned to bottle up their fear and anger and not communicate it.
Your Brain 101
In order to understand the potential risks of controlled crying, it is necessary to have a basic understanding of how our brains detect and take action in response to danger. Don’t worry about the fancy names for brain parts, just try and picture the gist of what happens.
Information we observe through our senses arrives at a part of the brain which receives and distributes messages like a central post office (the thalamus).
Messages arrive and the post office works out where they should go and distributes them to the correct addresses in the brain.
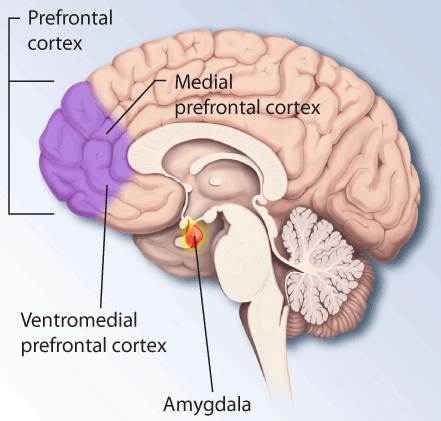
When your central post office receives information, one of the things it does is check whether we should be happy, angry, run away etc. It does this by sending messages to a part of your brain which functions as an automated alarm system (the amygdala):
and a more sophisticated security intelligence agency (the prefrontal cortex):
If your automated alarm system (amygdala) detects you are in the presence of something dangerous, it broadcasts a warning to the commander of your defence force (the hypothalamus):
The commander of your defence force mobilises all your body's energy for fight or flight – a process which is known as activating your 'stress response system'.
It does this by signalling your body to release the chemicals – the adrenaline rush - that make you feel your heart is in your mouth, your breathing gets faster, and makes you more alert. Depending on whether you are in control of the situation, these chemicals can make you feel terrified and anxious, or exhilarated. In addition to adrenaline, the adrenaline rush you feel also involves a chemical called cortisol.
You always have a bit of cortisol running through your body, because it's what makes you alert when you're awake. Your usual or 'base level' of cortisol is high just after you wake up, and gradually decreases over the course of the day, and is lowest at night when you are asleep. Cortisol is released when you are stressed to make you more alert in order to better react to the danger.
The burst of cortisol your body releases in response to stress is supposed to be short. When cortisol is released, your body also activates an internal timer which tells your brain to reduce cortisol levels about 20-30 minutes later. The parts of your brain which store memories keep an eye out for when cortisol levels drop sharply – then they think 'Ah, what just happened must have been important. I better store that away for future reference.'
This is why we remember dramatic or exciting events particularly vividly. However a very traumatic event causes us to keep producing cortisol, so levels don't drop for some time, and by the time they do, we have already lost most of the details from our short term memories, which is why the memory of really traumatic events can be blurry.
All the communication between your automated alarm system (amygdala) and commander of your defence force (hypothalamus) has already taken place while the security intelligence agency (prefrontal cortex) is still processing data.
Your security intelligence agency reacts with a smarter and more sophisticated (albeit a bit slower) response to danger, one that is based on vast amounts of information and memories and influenced by our conscious reasoning. If the automated alarm system is your emotional ‘instinct’, the security intelligence agency is your ‘emotional intelligence’. Your security intelligence agency (prefrontal cortex) is the part of the brain capable of overriding the automatic alarm system (amygdala) and telling your body – 'False alarm. It's ok, you can calm down now.' and for helping you detect and respond to the emotions of people around you.
The security intelligence agency (prefrontal cortex) has a left half and a right half, and your emotional reaction is influenced by which side is activated more. If the left side is activated, it tells you: 'Hey, that feels good. You want that. Go ahead.' If the right side is activated, it tells you: 'Careful, that's going to make you unhappy. Retreat.'
Brain scans reveal that different individuals have a tendency to process information with one side of the prefrontal cortex or the other, and this reflects their emotional style. Highly sociable, confident, risk-taking, or aggressive people tend to use the left side – these are people whose default response is to take action. By contrast, people who are anxious, depressed, or shy tend to use the right side – these are people who's default response is to be passive or withdraw.
Oh come on – how do they know that?
In one experiment, known as the 'Wada test', subjects were injected with a substance that temporarily dampened activity in their brain. When the substance was injected into the left brain, the subjects felt depressed. When it was injected into the right brain, the subjects felt euphoric. Numerous other studies have shown similar effects as a result of left-brain / right-brain damage (Harmon-Jones, Gable and Peterson). This led scientists to believe that:
- activity in the left prefrontal cortex is associated with pleasure / motivated behaviour;
- activity in the right prefrontal cortex is associated with sadness / depressed behaviour.
Because one half of the brain is activated more than the other in these situations, this is not symmetrical and so is known as 'cortical asymmetry'.
For the past decade, scientists have done experiments where they scan people's brains while relaxed, and while getting them to do things that will generate emotions (like thinking of a happy or sad memory, or looking at a picture of a spider). What they have noticed is that emotions are related to electrical activity in a part of the brain called the 'prefrontal cortex'. The prefrontal cortex is found on both the left and the right side of the brain. These experiments have confirmed that the kind of emotions experienced relate to which side of the prefrontal cortex is activated. When you have a happy experience the left prefrontal cortex lights up, and when you have a scary or sad experience, the right prefrontal cortex lights up (Harmon-Jones, Gable and Peterson).
They have found that depressed persons tend to have greater right frontal brain activity in general, but also that the amount of right frontal brain activity directly relates to the person's base level of cortisol. Remember, cortisol is one of the 'stress hormones'. When we are stressed, our bodies temporarily produce large amounts of cortisol, which helps us become very alert by helping us use extra sugar and oxygen (Davies et al). But when we are not dealing with a stressful event, our body still uses some cortisol to help keep us awake – we have higher levels of cortisol in the morning and less as the day goes on. The amount of cortisol our body produces when we are relaxed is known as our 'base level' of cortisol. What the studies indicate is that some people's 'base level' of cortisol seems to be set at a higher level, and that these people tend to feel depressed (Harmon-Jones, Gable and Peterson).
Having the right base level of cortisol seems to be important for healthy brain function. Both high levels of cortisol that spike excessively under stress and low levels of cortisol that fail to increase much under stress have been linked to problems. High levels lead to overreacting to stressful or novel situations and is believed to cause greater wear and tear on the body. On the other hand, cortisol has an important role in forming our memories, and too-low levels that do not react to stress can make it difficult to absorb and retain information. Children with too-low levels of cortisol are also more likely to show antisocial aggressive behaviour (Davies et al).
A person's base level of cortisol and right frontal brain activity when relaxed influences their reaction to positive or negative experiences. When watching a scary movie, persons who usually have high levels of right frontal brain activity responded with more fear and disgust. When watching a happy film, they responded with less joy. (Harmon-Jones, Gable and Peterson). In 10 month old babies, those with high levels of right frontal brain activity when relaxed tended to cry more when separated from their mothers (Davidson and Fox). In adults, higher levels of right frontal brain activity make it more likely that they will develop anxiety disorders over time (Blackhart et al).
But this is not to say that the left side of the brain is associated with all 'positive' behaviour and emotions and the right side with 'negative' behaviour / emotions. The left frontal side of the brain does not only light up with pleasure, it lights up with aggression. This seems to be because the anger in aggression is an emotion that is linked to motivation and action. If a person is angered in a situation where they are able to take action, their left frontal brain lights up more than if they are in a situation where they are unable to take action. In one experiment, people who disliked racism were shown pictures of unpleasant racist behaviour. This caused their left frontal cortex to light up. Some of the people had been told that after viewing the pictures they would be asked to write an essay on why racism was unfair and immoral – just knowing they would be expected to take action by writing the essay increased left frontal brain activity for these people (Harmon-Jones, Gable and Peterson).
More left frontal activity when relaxed is associated not only with more sociable behaviour and less fear of new situations, but with thrill-seeking and risky behavours in young adults, particularly young men (Santesso et al).
Following from this, how the brain responds is affected by whether we are able to take action or whether we feel helpless or restrained. People who are sitting upright have greater left-brain activity when they are insulted than people who are insulted when they are lying down. Similarly, people who are confrontational when angry have more left-brain activity, but those who tend to internalise their anger because they fear social disapproval have comparatively more right-brain activity when they feel angry. Similarly, people who are asked to envision an occasion when something good will happen to them have higher left-brain activity when the scenario involves them actively choosing behaviour that leads to them achieving the happy outcome (eg. work hard to receive a promotion) than when the happy outcome is out of their control (eg. winning the lottery) (Harmon-Jones, Gable and Peterson).
A mid-range increase in cortisol appears to help store events in our long-term memories. If the cortisol response is too high or too low, the memory is not stored properly. The chemistry of exactly why this happens is complex, but here is an attempt at a plain English explanation: Essentially brain cells have two parts that sense cortisol – one sensor sends a message that quickly makes you alert, the other sensor responds more slowly, telling the cortisol to go back to normal levels. When cortisol drops after a spike, this tells the brain that what just happened is important to remember. If cortisol is remains high, the memory isn't stored, but if cortisol is too low no spike is detected and the brain thinks that what happened is too unimportant to bother remembering (Oitzl et al). This explains why in a study of 3 month old infants, those with moderately increased cortisol learned and remembered that kicking moved a mobile, but those with very high or very low cortisol responses did not seem to remember the mobile a day later (Thompson and Trevathan).
In another experiment, 3 month infants who were placed in a novel situation only showed the ability to remember new knowledge if their cortisol levels had fallen about half an hour after the stressful event (Thompson and Trevathan), illustrating that it is necessary for the cortisol level to fall in order to remember new information.
Your Baby's Brain 101
You can think of your baby's brain like a new computer – but it's not just missing a lot of data compared to an adult brain, it's also missing crucial 'software'. The underlying 'hardware' is there – babies are born with the same number of neurons (brain cells) as an adult brain, but very few of the neurons are connected (Parsons et al). The connections are how knowledge, skills, and thought patterns are stored in our brains. Your baby’s brain triples in size in the first two years as a result of these connections being laid down (Eliot).
Obviously, your baby still has to learn the 'software' it needs to walk, talk, read, drive a car etc. But what you may not realise is that your baby also has a much more primitive operating system than you. If you have Windows 7, your baby is still using DOS – and what's more, he doesn't really understand how it works.
Your baby is born with a fairly functional amygdala (automated alarm system) and hypothalamus (defence force), but her prefrontal cortex (security intelligence agency) does not even start to show electrical activity until around 6 months after birth (Eliot) and does not develop enough to be basically functional until about 12 months after birth. Even then it continues to mature for many years (Parsons et al).
Development of the amygdala occurs in the two years immediately following birth, and its healthy development seems to depend upon the baby having reciprocal social interaction (Detweiler et al). Separation anxiety emerges as the amygdala begins a more advanced stage of development (Detweiler et al). By contrast, the prefrontal cortex (security intelligence agency) is still quite immature right up to adolescence, where it undergoes significant development (Detweiler et al). Interestingly, the amygdala becomes hyperactive during adolescence, and it takes some time for the prefrontal cortex to develop enough to allow an adolescent to regulate this new level of activity. In particular, it is very difficult for adolescents to switch off the feeling that they are being negatively evaluated by others (Detweiler et al). Myelination of the prefrontal cortex does not occur until late adolescence (Detweiler et al). Myelination means myeline grows along the neural pathways, making them work faster and more effectively (Siegel).
Emotional learning can take place before processes in the cortex is developed (LeDoux, p161). This is why your baby can develop associations with pleasant / unpleasant things, even before they can reason or understand cause and effect. So, your baby can become visibly excited by being placed in a feeding position and the smell of breastmilk/formula, even though the baby doesn’t reason ‘I’m about to be fed’ - they just sense ‘This is good!’
The fact that simple associations with fear can be formed have been shown by placing rats in a box, playing a tone, and giving them a mild electric shock. They come to associate the tone with the shock and be afraid of it, but they also associate the box with the shock and become afraid of that (LeDoux, p167). In another example, a human patient who had lost the ability to consciously create or access new memories was pricked with a tack upon shaking hands. Afterwards, she became reluctant to shake hands, even though she was unable to remember what she was afraid of (LeDoux, p181). These simple associations are formed using the amygdala, and mean that you can be thrown in an emotional state of fear without any conscious awareness of why it affects you. The only way to get rid of this kind of emotional reaction is to repeatedly experience the thing that triggers your emotion without any negative consequence – over time, this retrains your unconscious brain as to how to respond – although unconscious fear memories are tenacious and retraining may be difficult (LeDoux, p203).
A little baby under stress physically feels the emotion (heart rate increase, more alert, comfort or discomfort) but does not consciously recognise their comfort or discomfort, will never consciously remember it, and lacks the part of the brain needed to consciously calm themselves down (Eliot). Babies under about 6 months do not 'expect' a particular response from a caregiver. They smile because they are instinctively programmed to do so, not because they are thinking 'wow, I'm so happy!' They cry because they are uncomfortable and crying is their instinctive reaction when in discomfort. They calm down when their discomfort is alleviated – usually because of the action of a caregiver, but sometimes because of familiar pleasant sensations such as that produced by sucking or swaddling.
The correct translation of a wailing 4 month old baby then appears to be:
4 MONTH OLD BABY
The amygdala and hypothalamus are from an evolutionarily earlier part of the brain called the 'reptilian brain' – so it is no surprise that it puts your young baby's emotional IQ roughly on par with a crocodile (NB: this is a metaphor to help you picture the situation - I have no idea what the actual IQ of the average crocodile is). It also takes a lot of training and development for the prefrontal cortex to override the reptilian brain when we are upset. Hence, even by around 6 months when your baby starts to be capable of recognising mum as a source of assistance in times of emotional distress, their thought process is very primitive. A 7 month old baby will learn to cry to bring their caregiver to them, but impulse control is very low and the ability to deliberately employ other strategies is limited. That said, a baby over 6 months who is always ignored will eventually give up crying out for their caregiver as they will have learned it is pointless.
7 MONTH OLD BABY
The theory of controlled crying says that when you don't provide assistance to the baby to calm down, they stumble across alternative soothing techniques such as thumb-sucking, allowing them to soothe without a caregiver's assistance. This, they suggest, is why it can work with babies as young as 4 months old.
However, there is an alternative explanation as to why controlled crying leads to self-settling, and that is that the stress remodels your baby's brain, leading them to adopt withdrawn, passive behaviour.
Your baby's brain is like playdough
During the first two years of life, your baby's brain undergoes enormous development, sprouting more connections than the adult brain, then pruning these back, then abandoning old connections and creating new ones (Parsons et al). If your baby's brain was a house, then it would be like a home renovation show on crack. In science-speak it is said that your baby's brain has significant 'plasticity', which basically means it is capable of being modelled and remodelled – like playdough.
There is increasing evidence that the stress experienced by a baby during the first few years of life can change the way their brain develops. In extreme cases of psychological neglect, where children were fed, clothed, but otherwise left to cry and/or entertain themselves (eg. the infamous Romanian orphanages) children not only had poor intellectual development but actually had stunted physical growth. The intellectual and physical damage was permanent. Note that these children were kept sheltered and well fed.
No one is suggesting that controlled crying methods amount to that kind of extreme neglect (at least, I hope no one is, since that would be inaccurate and very unfair). There is a big difference between letting your baby cry on occasion, and ignoring them all the time. However, the extreme neglect cases do illustrate the point that what you do with very young babies can influence how their brains and bodies function for life.
The evidence suggests that a person's cortisol levels are set in response to the level of stress experienced in early life. Frequent moderate stress is adapted to by setting the body to release less cortisol when it encounters that particular stress. This is known as becoming 'habituated' to the stress, and is the reason why it might be scary to abseil the first time, but after several times most people get used to it. However, babies' primitive, plastic brains don't know to just modify the reaction to a specific stressful event – instead they cope by lowering cortisol levels generally, and reducing the amount of cortisol generally released. This allows the body to react less to stress, reducing discomfort, but also reduces the person's ability to feel emotions, detect and respond appropriately to the emotions of others, and impairs the ability to remember new information – and this effect continues for life.
Even worse, if the baby finds the stress too extreme and cannot cope, their stress response system malfunctions by becoming perpetually in a state of high alert. Base levels of cortisol become high and cortisol responses to stress are extreme and prolonged – essentially putting the person at high risk of developing an anxiety disorder or depression.
And how do they know that?
A basic understanding of children’s brains have been derived from brain scans of living children, and autopsies. Specifically, scientists have studied adults and older children who were known to have been abused or neglected in early childhood, and compared their brains and reactions with ‘normal children’. They have also done brain scans and measured cortisol levels of children and adults under various kinds of emotional influences, and performed controlled experiments with rats and monkeys where they study the effects of depriving them of maternal attention during early life.
At first the results of the studies were confusing. Children who grow up with parents who are unavailable have been shown to have higher levels of cortisol, as do children who grow up with physical and sexual abuse. However, other children who are exposed to high levels of stress, such as high levels of conflict between parents, have been shown to have too-low levels of cortisol (Davies et al, Carpenter et al).
However, it is now recognised that there are two common reactions to frequent stress - becoming overly ‘sensitised’ to stress (feeling constantly anxious and overreacting to stress), and becoming ‘habituated’ to stress (switching off to the stress).
The reason why there are two kinds of reactions is that frequent stress causes chronic exposure to cortisol, and this can actually remodel parts of your brain, but different parts are remodelled in different ways.
Chronic exposure to cortisol can make the amygdala (automatic alarm system) more sensitive to threats, but make the hypothalamus (commander of defence force) less responsive, and reduce cortisol receptors in the prefrontal cortex (emotional intelligence centre) (Loman and Gunnar).
Which way we react seems to depend on whether the repeated stress is overwhelming (which results in sensitisation) or just unpleasant (results in becoming habituated). This means that reactions will vary depending on the intensity and duration of the stress and the context in which the stress occurs. It also seems to depend on the individual.
The idea that some children are at special risk of developing problems down the track is emphasised by a study that showed four year old boys who withdrew from social situations were a little more likely to have higher cortisol levels, but if they had also shown a 'difficult' personality at 9 months of age they were substantially more likely to have higher cortisol levels at 4 years of age. Just to keep this all in perspective though, in a sample of 41 males, cortisol levels alone predicted 4.6% of withdrawal, personality at 9 months predicted 9% of withdrawal, and combined personality and cortisol predicted an additional 14.1% of withdrawal (Perez-Edgar et al).
Studies on how and whether humans habituate or sensitise to particular kinds of stresses have found that the kind and intensity of the stress matters, as does the individual (Wüst et al). In a study of 54 young men, cortisol levels were assessed over several weeks as subjects were required to do a moderately stressful maths and language task. The study found that for the majority of people, they found the task progressively less stressful as they got used to it (52%), but for some participants there was no change and for 16% of participants the task became progressively more stressful. Those who habituated to the task well were those with greater cortisol reactivity to stresses in general (Wüst et al).
It also may depend on gender, as women tend to have more right frontal brain activity and higher cortisol generally - so females may be more prone to sensitisation and males to habituation. One study found that pre-school age children with context inappropriate anger (children who become angry or aggressive without provocation, for example) have lower cortisol levels generally, and that this was particularly true for boys, who also had a lesser decrease in cortisol over the course of the day (Locke et al). Lower cortisol levels with a lesser decrease has been reported for children in stressful early environment (Gunnar & Vazquez).
In rats, a stressful situation early in life (for example, prolonged absence of the mother) caused higher base cortisol levels early in life, and very low base cortisol levels in mid-life . The rats exposed to the early stress were not able to absorb new information very easily, as tested by their performance in a novel maze. When given the opportunity, they were also more likely to give themselves amphetamines, moderate to high amounts of alcohol, and morphine than rats that were not stressed in early life (Oitzl et al).
How stressful is it for a baby to be left to cry?
Amazingly, given it is a common parental practice, no one appears to have studied what happens when a baby is left to cry - in terms of measuring their brain activity or cortisol levels.
We can look at how much a baby's cortisol rises in response to an event to find out how stressful the event was to the baby. One study tested how 6 month olds reacted when their mothers stared at them with disinterest. This has been shown in other studies to appear to distress infants of this age. In this study, the baby's reactions and cortisol levels were measured. What they found is that, of the babies who reacted, those babies who appeared to be sad had a greater cortisol reaction, but those babies who appeared to be angry did not. This fits with other studies on cortisol and right-brain activity which shows they are linked to withdrawal, sadness, and feeling helpless, whereas anger is an active response associated with the left brain (Lewis and Ramsay).
At six months, babies who have exhibited sad or withdrawn behaviours when approached by a stranger have very high levels of right frontal brain activity as they were approached. Those who had extreme levels of right frontal brain activity generally had high base levels of cortisol, and those with extreme levels of right frontal brain activity during the test had higher levels of cortisol. For those babies who displayed extremely noticeably sadness, right frontal brain activity and cortisol levels were also very pronounced (Buss et al).
In even younger babies at 4 months, the babies were rewarded with smiling faces and music when they moved their arm a certain way. After they had learned to move their arm to obtain the reward, researchers measured what happened when they stopped getting the reward in response. Again, sadness predicted elevated cortisol but anger did not. Upon learning they no longer had the power, babies typically moved through the emotions of surprise, then anger, then sadness – at which point they reduced and then gave up their efforts. The babies who showed more angry responses were liable to persist in trying to obtain the role in the face of adversity, whereas the babies that showed sadness tended to give up. The study suggested that a cortisol approach to goal blockage does not occur until efforts to overcome the obstacle are not effective (Lewis and Ramsay).
In newborns, increased cortisol was found following a heelprick, and following a routine medical exam (Gunnar and Donzella). In 9 month olds, cortisol increased during separation from the mother, increased if placed with a substitute caregiver who ignored the infant, but did not increase if a substitute caregiver looked after the infant responsively when the mother was away (Thompson and Trevathan). In baby monkeys, separation from the mother also tended to increase cortisol (Gunnar and Donzella).
Temporary decreases in cortisol are caused by relaxing, pleasurable activities. Car rides and mother-baby swimming sessions have been shown to reduce cortisol for babies between about 6 and 18 months (Gunnar and Donzella). Newborn babies can become used to mild stresses, such as medical exams and show lower levels of cortisol as medical exams are repeated, but become increasingly distressed by strong stresses, such as a heelprick test when this is repeated (Gunnar and Donzella).
Cortisol reactivity starts out very high in a newborn, causing spikes about 5 times higher than in a 6 month old, and about 10 times higher than a 2 year old (Jansen et al). There is a substantial amount of data showing that babies have strong cortisol reactions to acute pain, such as a vaccination needle. However, there is very little data on the effect of psychological stress such as that caused by being separated from a mother. Tests have only been done on babies 9 months or older, and they showed weak reactions to a 30 minute separation at around 9 months (although comparable to that for a vaccination), and little reaction for toddlers (Jansen et al).
By about 12 months babies develop much greater control over their cortisol levels – after 12 months, most children do not have cortisol reactions for separations from their caregivers (Gunnar and Donzella), even though many would still be exhibiting behaviour that suggests separation anxiety. Children's experiences as well as their individual personalities also start to shape cortisol responses as they get older – children with insecure attachments show unusually high cortisol spikes in response to injections at 15 months (Gunnar and Donzella). A number of studies have shown that shy babies and toddlers, as well as easily frustrated babies and toddlers, have unusually elevated cortisol in response to novel situations only if they also have insecure attachment (Gunnar and Donzella). Studies of orphans from orphanages with extremely poor quality of care who were adopted out into loving families between 8 months and 3 years of age showed that they still had higher than usual levels of cortisol when they were 6 years old – the older the child was before they were removed from the orphanage, the higher their level of cortisol at age 6 (Gunnar and Donzella).
Given that secure attachment develops when babies are given sensitive, responsive, consistent care, these studies suggests that such care during the first few years of life helps babies to develop the ability to appropriately regulate their own cortisol reactions. But if babies do not receive the responsive care necessary to develop secure attachment, they are at risk of developing problems regulating their stress reactions, particularly if they are naturally shy and fearful. It is also interesting to note that these babies and toddlers may cry and carry on in response to a stressful event, but if a comforting caregiver is present when they do so, their physical stress reaction is still being kept under control. In a study of 64 infants about 3 months of age, the sensitivity of mothers during a mild stressful experience was found to be able to significantly aid in the infant's ability to lower their cortisol levels after the stressful experience (Albers et al).
If you do want to teach your child (older than 6 months) to feel comfortable with being separated from you, it is worth remembering that when your child has not had much sleep, the connection between the amygdala and the prefrontal cortex does not work very well. Instead, the amygdala tends to directly link to the parts of the brain that work sub-consciously (Jan et al). This strongly suggests that a tired baby is least able to recognise his emotions or control his behaviour – his response will be mostly on autopilot.
But if it were that harmful, wouldn’t we see problem children everywhere?
Yes and no. There are lots of other influences on your child's psychological development than the way you approach sleep. For example, one study found that giving children the opportunity to observe positive, intimate relationship models is an important ingredient in children developing the ability to form close, positive friendships by primary school age (Lucas-Thompson and Clarke-Stewart). A study of 44 toddlers looked at whether there was any effect from regular strategic use of strategies of maternal unavailability (crying it out / locking a child in their room / deliberate ignoring the child etc). The study found that toddlers who had been subject to deliberate unavailability had higher levels of base cortisol than toddlers whose behavioural difficulties were approached in other ways. By contrast, toddlers who were smacked for misbehaviour did not have elevated base cortisol, but had greater reactivity to stressful situations (Bugental et al).
One important influence is the child’s own biology. The picture the studies suggest is that for most children the stress has to be pretty extreme to cause problems, but for a small percentage of children even small amounts of stress can cause problems.
Evolutionary biologists have pointed out that the level of anxiety-related disorders prevalent in human society ought to be fairly low, since coping with fear is a natural and normal part of our evolved behaviour. The rate of anxiety disorders in modern societies is particularly high, which is strange, given that there are less serious dangers to face in the modern, developed world (Grinde). For example, the annual cost of anxiety disorders during in the United States during the 1990s was approximatley US$42 billion (Detweiler et al). Given that very early childhood seems to be a time when the brain and body develop our 'usual' approach to anxiety, this is a logical place to look for the scary experience(s) that would set usual levels of anxiety at higher levels. It is a striking feature of contemporary, Western child-rearing practices that babies spend comparatively little time in physical contact with their caregivers, and from a very early age many are deliberately and frequently left to cry in order to teach them to settle without parental assistance. It has been argued that perhaps it is these practices, which are known to cause the babies distress, are responsible for shaping our brains to have higher anxiety levels (Grinde).
Children at special risk of developing problems
In studies of infants of depressed mothers, it has been found that these have greater right frontal brain activity from birth (suggesting an effect that is either genetic, or occurs as a result of the environment in utero), however if their mothers tend to be very interactive with them they shift towards greater left frontal activity. On the other hand, if their mothers are withdrawn and emotionally distant towards them, their right frontal brain activity becomes stronger (Diego et al).
Regardless of whether their mothers are depressed, insecurely attached infants tend to show higher right frontal brain activity than securely attached infants, but infants of depressed mothers show even higher readings. This tends to suggest that maternal depression does not determine brain assymetry, but rather that it is a risk factor, perhaps because it may be harder for depressed mothers to interact with their babies in a consistent and emotionally available way, and that puts those babies at greater risk of developing insecure attachment (Dawson et al).
While babies with very sad reactions tend to have very high right frontal brain activity, it is not the case that the less sad a baby looks, the less right frontal brain activity they have. This may indicated that different babies display their inner feelings with different levels of intensity, which suggests it is important for a carer to get to know a baby well in order to judge what their crying means. This is further emphasised by another study which involved testing babies at 3 month immunisations. The study found that soothing the baby with a pacifier and glucose did not reduce crying time but it reduced cortisol levels (Mörelius et al.) A meta-study of babies and pain found that it is difficult to use crying as a measure of how much pain a baby is in, as pain-related behaviours differ vastly from baby to baby (McGrath).
Allostatic load
“Allostasis refers to the process by which biological 'set points' in homeostasis are altered to generate physiological resources necessary to promote survival in the face of environmental stress and challenge. However, in highlighting the operation of allostatic load, successive cycles of allostasis engendered by repeated exposure to environmental adversity have been theorized to result in wear and tear on the body that undermine the integrity of multiple domains of functioning.” pp918-9 Davies et al
As I have already discussed, when we are stressed our bodies put energy where it is most needed and neglect those parts of the body that aren't required to deal with the immediate stress. But what happens if we are stressed too frequently? The theory of allostasis says that when we get stressed all the time, we get used to running in overdrive, and this causes wear and tear on our bodies. It also makes it hard to 'switch off' in periods of relative calm and this makes it difficult to regulate our bodies as per normal. Scientists believe this is why ongoing stress leads to high blood pressure, a poor immune system, a tendency to put on weight etc (Evans).
A short but quite intense stressful experience (eg. a steam burn) is believed to have less harmful impacts than regular, moderate stress. The exception is that if you genuinely stop finding the experience stressful (Evans). So, if you have to speak in front of a crowd, you might find that stressful the first few times then find it gets easy and you stop worrying about it. In fact, you might even start to feel happier and more confident because you have conquered that particular stress. When you genuinely stop feeling stressed about something, it does not continue to cause harm to your body. But if you keep being stressed every time you speak, and you have a job where you have to do a lot of public speaking, over time you will build up your the 'allostatic load' and cause wear and tear on your body. It is also likely that you will lose confidence as you feel increasingly helpless in your ability to deal with the stress.
Allostatic load is increased by one-off serious stresses, but also by a combination of ongoing moderate and minor stresses (Evans). So, if your baby drowns in the bathtub, that is an 'acute stress' which is likely to increase allostatic load. But if you never quite get enough sleep, deal with a bitchy co-worker, your washing machine keeps breaking down, you struggle to pay the bills, and you are constantly being criticised by your mother in law – over time these cumulative stresses can also significantly increase your allostatic load.
Studies have shown that the more serious and / or ongoing stresses a child is exposed to over time:
- the lower their self-confidence and belief in their own competence, reducing their ability to persist in the face of adversity;
- the less able they are to control their own behaviour;
- the more likely they are to store excess body fat;
- the more likely they are to have raised blood pressure in response to stress; and
- the higher their base level of adrenaline and cortisol (Evans).
Prolonged exposure to cortisol has been found to be linked to accelerated aging, increased susceptibility to illness, and cognitive impairment (Luecken and Lemery). Young adult women who have more right frontal brain activity have been found to have less effective immune systems (Kang et al).
However, it has also been shown that having a primary carer who is caring and responsive can protect children from having their allostatic load increased by significant stress (Evans et al).
Attachment
Attachment behaviour develops around 5-6 months. Attachment behaviour occurs when a baby starts to strongly make a point of directing behaviour at their primary caregiver, and starts to exhibit separation anxiety. The fact that attachment behaviours are a normal and healthy part of infant development was first described by J Bowlby in the 1960s, and this proposition has been supported by so many studies that it is widely accepted in the medical and psychological literature as a key feature of early child development (see review by Parsons et al).
Numerous studies have found that developing a 'secure attachment' as a baby leads to greater confidence and independence less behavioural problems, and better social interactions, as the child gets older (Detweiler et al). By contrast, insecure attachment puts a person at risk of developing a wide variety of mental disorders (Buccheim et al). Children with insecure attachment styles are twice as likely to develop anxiety disorders as teenagers as children with secure attachment styles (Detweiler et al.)
Babies and toddlers with secure attachment still frequently become distressed when separated from mum, but they are basically happy to see her and interact with her comfortably when she returns. By contrast, various insecure styles of attachment involve the child ignoring the parent upon return, responding to the parent with anger or ambivalence, or excessive clinginess on return. Nearly all infants become attached to parents, but not all become securely attached.
There are two accepted psychological tests for measuring attachment – the 'Strange Situation' test, and the 'Attachment Q-Set'. The Strange Situation involves the caregiver leaving the child in a room and a stranger entering the room, before the caregiver returns. The child's reactions to the parent leaving, to the arrival of the stranger, and to the return of the parent are observed. The Attachment Q-Set is a parental questionnaire. These tests are used with infants after attachment has developed (Parson et al).
Wikipedia has a useful, brief summary of secure attachment behaviour and the three types of insecure attachment behaviour (avoidant, ambivalent, and disorganised).
Secure attachment is promoted by:
- availability of the caregiver or caregivers to whom the child is becoming attached;
- prompt and appropriate responses to infant cues;
- assuming the child has coherent (although not necessarily well-informed) opinions, and expressing back to the child with a fair degree of accuracy what the child is thinking / feeling (eg. 'Wow, you really like chicken!' 'You want that toy.' or 'You hit your brother because you were angry.') This is known as 'mind-mindedness' (Parsons et al).
Statistically, mothers of ambivalently attached infants are less sensitive and responsive to their infant's cues when in a situation where there are multiple demands on their attention (Harel and Scher). When a child is unhappy for long periods of time, and is not assisted by their caregiver to get out of the unhappy state, they have an increased risk of developing psychological problems (Schore in Harel and Scher).
Secure attachment actually increases the chances of being a better sleeper in the long run, unless the baby becomes extremely detached from their caregiver and emotions generally (avoidant attachment). One study indicated that avoidant and securely attached children were good sleepers. Children with 'disorganized' attachment were slightly worse, but children with ambivalent attachment were much more likely to be poor sleepers (Morrell and Steele). Ambivalent attachment results from low or inconsistent maternal availability – babies who are unsure whether maternal comfort will be forthcoming learn to overexpress attachment behaviours to increase the chances of their attachment needs being met. An ambivalently attached infant is very distressed on separation from a mother, and clingy and angry when the mother returns. It is likely that attempts to leave a child with ambivalent attachment to cry it out would fail, and the attempt would only make the ambivalent attachment behaviour worse.
Another study of toddlers found that 100% of the toddlers with sleep disorders had insecure attachment, while on 57% of the toddlers without sleep disorders had insecure attachment (Benoit et al). Infants who were able to comfort themselves with a toy or blanket without crying out have also been found to have more secure attachment (Middlemiss).
Responsive parenting, where a parent responds promptly and sensitively to a child's needs, has been shown to improve language acquisition and social cooperation, and less distress and greater problem-solving ability when required to interact in a novel situation with a stranger (Landry et al). Good attachment is believed to develop when infants have attachment figures (typically their parents) who are 'available to them on a one-to-one basis, who are attuned to them in times of excitement and distress, and available to protect them when they were in danger. Attachment theory suggests that the separation from one's attachment figure that occurs in going to sleep is a separation that provokes anxiety, as does the absence of the attachment figure during night awakenings (Priddis).
A 2000 Israeli study looked at 94 12 month old infants found that the percentage of 12 month old infants who are 'night wakers' is higher for attached babies than babies with insecure attachment behaviour (Scher, 2001). An Australian study of 65 first-time mothers with infants between 7-19 months found that mothers with lower sensitivity were more likely to have poor sleeping infants and seek assistance for their infants sleep behaviour. Two of the mothers from this study with poor sensitivity and babies with severe sleep problems were then invited to participate in a six-session program where the mother was encouraged to observe and respond to their children's expressed needs to be close to them and be comforted, as well as to allow the child to explore. In both cases, the amount the mother improved in sensitivity as a result of the program was the amount the infant improved in sleeping pattern (Priddis).
Secure attachment at 18 months has been showed to be linked to better mother-child interaction in middle childhood. A longitudinal study of 45 infants observed at 18 months and then at 7 years found that when the baby-mother pairs had secure attachments, they had more positive interactions at 7 years after a brief period of separation. The securely attached 7 year olds and their mothers tended to greet each other with delight, talk about what they had been doing, then enjoy playing a game together. The insecurely attached pairs were characterised by children with negative attention-getting behaviour, and mothers who either ignored their children, criticised them, overwhelmed them, or swung between extremes of this kind of behaviour (Easterbrooks et al). Babies with good attachment seem to develop this when mothers are responsive to their attempts at communication and help them calm down when they are distressed (Easterbrooks et al).
Another study looked at maternal sensitivity and control in Finland. A study of 75 mother-child pairs over two years found that low maternal sensitivity and high levels of maternal control at 2 and 4 months predicted low child cooperation in those same children at two years old. Sensitivity means responding to the child's signals consistently and appropriately, to help the infant stay comfortable, reduce the baby's distress, and helping the baby to calm down when he or she gets worked up (Kemppinen et al). Maternal control means when an overly-pushy style where mothers attempt to force babies to comply with their own controlling behaviour – for example, by forcing the child to interact when the child is not interested, intrusive poking and manipulating the baby's body, or covert or overt anger towards the uncooperative baby. Moderate levels of maternal control that sensitively decrease over the first 2 years of the child's life were not found to have negative effects (Kemppinen et al).
One study of 215 children followed from 15 months until the age when the left home and went to kindergarten. It found that children who were wary of novelty at 15 months were likely to have difficulties in starting kindergarten, but that of these children, those with mothers who displayed high sensitivity were less likely to have difficulties starting kindergarten. For those 15 month children who were not wary, maternal sensitivity had nothing to do with difficulties in starting kindergarten (Early et al). What this suggests is that when a child is particularly anxious and clingy at 15 months, responding with patience and sensitivity rather than pushing the child to become independent is more likely to encourage independence as the child gets older.
An American study of 142 children monitored their sleep for a week at grade 3 and then again at grade 5 found that children who were more emotionally secure were significantly less sleepy during the day. Children's greater emotional insecurity with respect to family relationships had greater subjective sleep problems, poor objective sleep quality, and reduced sleep duration. In particular, the study found that a good level of emotional security predicted better sleep, but better sleep did not predict emotional security (Keller and El-Sheikh). Good attachment is only one factor in promoting emotional security in older children – family discord also has a big impact. However, what this highlights is that for most children 'sleep training' only addresses the symptom of the problem, and in fact may exacerbate the insecurity which is the problem's underlying and long-term cause.
Sensitivity means not only assisting your child when they need assistance, but backing off when your child needs a break. Because of 'attachment parenting' is associated with co-sleeping and babywearing, many people think of it as having the baby physically attached to you at all times. But really, attachment theory is not about physical contact – although that may be one way of keeping you and your child connected. It is about sensitivity, responsiveness, and consistent availability.
That said, hugging and touching produces oxytocin. Oxytocin is a chemical found in the human body that increases trust, reduces your physical and emotional response to stress, increases your ability to be sensitive to others' feelings and generally makes you more sociable (Buccheim et al). In a study of 26 adult males with insecure attachments, administering oxytocin led to a small but noticeable increase of most of those subjects' tendency to show securely attached behaviour. This was most true for those subjects whose attachment style was 'preoccupied' (Buccheim et al).
PND and Crying it Out
While we all know the baby is not the only person in a mother-infant relationship, sometimes the baby is not the only vulnerable person either. This is particularly true when mum has PND. Is there a more compelling case for controlled crying with PND?
I don’t think there is a straight-forward answer. There is an Australian study which suggests a program of controlled crying resulted in less depression for the mothers once their baby was sleeping better, at least in the short term (Hiscock et al). However, the study did not control for whether the effect was caused by the one-on-one support and ‘confidence boost’ that the instruction on controlled crying training had on the mums, so it is difficult to tell whether cc itself was what made the difference. That said, severe sleep deprivation is known to cause cellular stress. It seems to put people at a higher rate of depression and increase susceptibility to other stresses (Jan et al).
The other side of the coin is that bubs of depressed mums are already more likely to be at risk of developing problems as a result of stress - both anxiety disorders and difficulty developing secure attachment. Programs that encourage depressed mothers to be more sensitive to their infants' cues have been found to improve the chances of developing secure attachment. Secure attachment at 10 months led to less behavioural problems at 2 years (Cheng et al). Hearing your infant cry is not exactly a relaxing experience to ‘treat’ a depressed mother - it affects the level of cortisol in your own body. Parents who hear their own infants cry have been found to have significant raised levels of cortisol that increased the longer the infant cried (Mörelius et al.)
But haven’t they shown that crying methods are ‘safe’ after 6 months?
The evidence here is pretty sketchy indeed. Here it is summarised for your consideration:
In a 1991 British study looked at 63 children between 6 and 24 months (France). This is one of the studies that is often cited as showing sleep training is beneficial, so I thought I would look at it in detail.
The children studied were divided into 3 groups – those seeking treatment for sleep difficulties and who adopted sleep training, those who weren't seeking assistance but who had significantly disrupted sleep, and those who were not seeking assistance and did not have significantly disrupted sleep. Children's daytime behaviour was rated by parents using questionnaires prior to sleep training (or no sleep training for a control group), on the third day, after six weeks, and during follow-up (which occurred at either 6 months, 18 months, or 30 months). Children's behaviour was not independently observed by the researchers.
Firstly, this study suggests sleep training 'works', in the sense of reducing sleep disruptions at night. Prior to treatment, infants with severe sleep disruptions scored 11.0 on a parentally rated sleep disruption test, which was reduced by 6 weeks of sleep training to 4.4, and at follow-up found to be 2.6 (2.8 is considered average for a good sleeper). The poor sleepers in the control group only started with a score of 7.1 but this only reduced to 6.2 over 6 weeks, and to 5.8 by follow-up.
Looking at the actual study showed that sleep training appears to benefit parents who find their children's sleep distressing to the point they seek intervention, and that the parents who with poor sleepers who did not find their children's sleep distressing were actually just fine without sleep training.
The study found that parents who sought treatment for sleep difficulties rated their children's attachment security as worse prior to intervention (28.6), and much more positively three days into sleep training (32.2) and six weeks later (36.2). Parents who did not seek or receive treatment started with significantly better attachment scores (33.7 for normal sleepers, 34.8 for poor sleepers). This held steady for the good sleepers without intervention (33.7 at 3 days and 32.1 at 6 weeks) and somewhat improved for poor sleepers without sleep training (39.8 at 3 days and 36.9 at 6 weeks).
Parents who sought sleep training had babies they found significantly 'agreeable' (24.1) and less 'likeable' (20.3) than parents who did not seek sleep training (28.3 agreeableness and 22.1 likeability for good sleepers, and 27.6 agreeableness and 24.3 likeability for poor sleepers not seeking treatment). Likeability and agreeableness improved fractionally for the group that received sleep training, and decreased fractionally for the group that did not. At 6 weeks, the sleep training group had a modest improvement in likeability scores (20.3 to 21.7) whereas the poor sleepers who did not have sleep training had a significant decrease in likeability (24.3 to 20.4), but at follow-up it was all much of a muchness (21.4 for sleep trained and 21.8 for non-sleep trained).
Parents who sought sleep training rated their babies as significantly more emotional / tense prior to training (15.7) than the controls (11.0 good sleepers, 9.5 poor sleepers). This emotionality was slightly reduced by sleep training (13.7) but had increased again at follow up (14.8), it increased slightly for the good sleepers without sleep training (to 12.7) and the poor sleepers without intervention (12.2), but still remained below the sleep training group.
One problem with this study is that the control groups did not have interaction except to fill out a survey, whereas the treatment group appeared to have been trained and supported in adopting a behavioural program to deal with their infant's sleep. The study is unfortunately not specific as to the methodology of the program or the control group.
More recently, an Australian study followed 328 mothers who reported an infant sleep problem at 7 months. These were divided into two groups – the mothers in one of the groups the 'intervention group' were invited to contact a health nurse to learn how to use a behaviour method to address the sleep problem. This was done with 1 on 1 advice from a nurse on how to perform a particular intervention. 53 families chose to use graduated extinction, 7 chose 'camping out', 20 opted for simple non-crying strategies such as a positive bedtime routine, and the strategies of the other 20 were not noted. Two years later, 27.3% of those from the intervention group reported sleep problems, whereas 32.6% of the non-intervention group. However, it should be noted that only 15.4% of mothers in the intervention group had maternal depression as compared to 26.4% of the non-intervention group. The way it was decided whether a sleep problem existed was to ask: “Over the last 2 weeks, has your child's sleep generally been a problem for you?” yes or no. Obviously, the answer to this question reflects parental perceptions and their thresholds of tolerance as much as it reflects their child's objective sleep behaviour (Hiscock et al).
The mothers in the intervention group indicated strong satisfaction with the behavioural methods they had chose, and when they were asked whether they felt it had had a negative or positive effect on their relationship with their child, most mothers felt the impact was basically neutral or slightly positive. Mothers also completed questions about their parenting style and their children's behaviour. These questionnaires indicated that the intervention group, even by their own admission, had a slightly less nurturing and very slightly harsher parenting style, but maternal reports of child behaviour were similar for both groups (Hiscock et al).
In an earlier part of this study, the researchers also considered the extent to which resolution of sleep problems assisted depressed mothers. It found that 2 months after the intervention depressed mothers in the intervention group had significantly more improvements than non-depressed mothers (Hiscock and Wake). One critic points out that this is a very unusual result, given that one would expect depressed mothers to not have as much improvement in sleep as they would be less capable of effectively implementing the sleep training. He suggests that it is possible that the cause of mothers reporting less sleep problems was the support and confidence given by the one-on-one training, and that this was more helpful and meaningful for the depressed mothers. Hence it may not have even been the sleep training which generated the improved results (Lipman).
Coming up next...
Effectiveness of non-crying methods.
References
Albers et al, 'Maternal behavior predicts infant cortisol recovery from a mild everyday stressor' (2008) Journal of Child Psychology and Psychiatry Vol 49(1), p97.
Benoit eg al, 'Sleep Disorders in Early Childhood: Associated with Insecure Maternal Attachment' (1992) Journal of the American Academy of Child Adolescent Psychiatry Vol 31(1), p86.
Blackhart et al, 'Can EEG asymmetry patterns predict future development of anxiety and depression? A preliminary study' (2006) Biological Psychology Vol 72, p46.
Buchheim et al, 'Oxytocin enhances the experience of attachment security' (2009) Psychoneuroendocrinology Vol 34, p1417.
Bugental et al, 'The hormonal costs of subtle forms of infant maltreatment' (2003) Hormones and Behavior p237.
Buss et al, 'Right Frontal Brain Activity, Cortisol, and Withdrawal Behaviour in 6-Month-Old Infants' (2003) Behavioral Neuroscience Vol 117(1), p11.
Carpenter et al, 'Effect of Childhood Emotional Abuse and Age on Cortisol Responsivity in Adulthood' (2009) Biological Psychiatry Vol 66, p69.
Cheng et al, 'The effectiveness of early intervention and the factors related to child behavioural problems at age 2: A randomized controlled trial' (2007) Early Human Development Vol 83, p683.
Chilton, Baby on board: understanding what your newborn needs in the first twelve months (2009, 2nd Ed.) Finch Publishing.
Chorney et al, 'The Interplay of Sleep Disturbance, Anxiety, and Depression in Children' (2007) Journal of Pediatric Psychology Vol 33(4), p339
Davidson and Fox, 'Frontal Brain Asymmetry Predicts Infants' Response to Maternal Separation' (1989) Journal of Abnormal Psychology Vol 98(2), p127.
Davies et al, 'The Role of Adrenocortical Functioning in Pathways Between Interparental Conflict and Child Maladjustment' (2007) Developmental Psychology Vol 43(4), p918.
Dawson et al, 'Autonomic and brain electrical activity in securely- and insecurely-attached infants of depressed mothers' (2001) Infant Behavior & Development Vol 24, p135.
Detweiler et al, 'Social Anxiety in Children and Adolescents: Biological, Developmental, and Social Considerations' (2010) Social Anxiety: Clinical, Developmental and Social Perspectives p223.
Diego et al, 'Withdrawn and intrusive maternal interaction style and infant frontal EEG asymmetry shifts in infants of depressed and non-depressed mothers' (2006) Infant Behaviour & Development Vol 29, p220.
Early et al, 'Maternal Sensitivity and Child Wariness in the Transition to Kindergarten' (2002) Parenting: Science and Practice, Vol 2, p355.
Easterbrooks et al, 'Infancy predictors of emotional availability in middle childhood: the roles of attachment security and maternal depressive symptomatology' (2000) Attachment and Human Development Vol 2, p170.
Eliot, What's Going On In There? How the Brain and Mind Develop in the First Five years of Life' (1999) Bantam Books, pp 292-95.
Evans, 'A Multimethodological Analysis of Cumulative Risk and Allostatic Load Among Rural Children' (2003) Developmental Psychology Vol 39(5), p924.
Evans et al, 'Cumulative Risk, Maternal Responsiveness, and Allostatic Load Among Young Adolescents' (2007) Developmental Psychology Vol 43(2), p341.
Grinde, 'An approach to the prevention of anxiety-related disorders based on evolutionary medicine' (2005) Preventive Medicine Vol 40, p904.
Gunnar and Donzella, 'Social regulation of the cortisol levels in early human development' (2002) Psychoneuroendocrinology Vol 27, p199.
Harel and Scher, 'Insufficient responsiveness in ambivalent mother-infant relationships: Contextual and affective aspects' (2003) Infant Behaviour & Development Vol 26, p371.
Harmon-Jones, Gable and Peterson, 'The role of asymmetric frontal cortical activity in emotion-related phenomena: A review and update' (2010) Biological Psychology Vol 84, p451.
Hiscock et al, 'Long-term Mother and Child Mental Health Effects of a Population-Based Infant Sleep Intervention: Cluster-Randomized, Controlled Trial' (2008) Pediatrics, Vol 122(3), pe621.
Jan et al, 'Long-term sleep disturbances in children: A cause of neuronal loss' (2010) European Journal of Paediatric Neurology Vol 14, p380.
Jansen et al, 'Cortisol reactivity in young infants' (2010) Psychoneuroendocrinology Vol 35, p329.
Kang et al, 'Frontal Brain Asymmetry and Immune Function' (1991) Behavioral Neuroscience Vol 105(6), p860.
Keller and Ek-Sheikh, 'Children's emotional security and sleep: longitudinal relations and directions of effects' (2011) Journal of Child Psychology and Psychiatry Vol 52(1), p64 (published online in 2010).
Kemppinen et al, 'The continuity of maternal sensitivity from infancy to toddler age' (2006) Journal of Reproductive and Infant Psychology Vol 24, p199.
LeDoux, The Emotional Brain (1998), Touchstone.
Lewis and Ramsay, 'Infant emotional and cortisol responses to goal blockage' (2005) Child Development Vol 76(2), p518.
Lipman, 'The limitations of randomised controlled trials for socially constructed interventions'
Loman and Gunnar, 'Early experience and the development of stress reactivity and regulation in children' (2010) Neuroscience and Biobehavioral Reviews Vol 34, p867.
Lucas-Thompson and Clarke-Stewart, 'Forecasting friendship: How marital quality, maternal mood, and attachment security are linked to children's peer relationships' (2007) Journal of Applied Developmental Psychology Vol 28, p499.
Luecken and Lemery, 'Early caregiving and physiological stress responses' (2004) Clinical Psychology Review p171.
McGrath, 'An assessment of children's pain: a review of behavioral, physiological and direct scaling techniques' (1987) Pain Vol 31, p147.
Middlemiss, 'Infant sleep: a review of normative and problematic sleep and interventions' (2004) Early Child Development and Care Vol 174, p99.
Mörelius et al., 'Stress at three-month immunization: Parents' and infants' salivary cortisol response in relation to the use of pacifier and oral glucose' (2009) European Journal of Pain Vol 13, p202.
Morrell and Steele, 'The Role of Attachment Security, Temperament, Maternal Perception, and Care-Giving Behavior in Persistent Infant Sleeping Problems' (2003) Infant Mental Health Journal Vol 24(5), p447.
Oitzl et al, 'Brain development under stress: Hypotheses of glucocorticoid actions revisited' (2010) Neuroscience and Biobehavioural Reviews Vol 34, p853.
Parsons et al, 'The functional neuroanatomy of the evolving parent-infant relationship' (2010) Progress in Neurobiology Vol 91, p220.
Perez-Edgar et al, 'Salivary cortisol levels and infant temperament shape developmental trajectories in boys at risk for behavioral maladjustment', (2008) Psychoneuroendocrinology Vol 33, p916.
Priddis, 'Tuned in parenting and infant sleep patterns' (2009) Early Child Development and Care Vol 179, p259.
Santesso et al, 'Frontal EEG asymmetry and sensation seeking in young adults' (2008) Biological Psychology Vol 78, p164.
Scher, 'Maternal separation anxiety as a regulator of infants' sleep' (2008) Journal of Child Psychology and Psychiatry Vol 49(6), p618.
Scher, 'Attachment and Sleep: A Study of Night Waking in 12-Month-Old Infants' (2001) Developmental Psychobiology Vol 38, p274.
Siegel, The Developing Mind: How Relationships and the Brain Interact to Shape Who We Are (1999) The Guilford Press.
Smaldone et al, 'Sleepless in America: Inadequate Sleep and Relationships to Health and Well-being of Our Nation's Children' (2007) Pediatrics Vol 119, pS29.
Thompson and Trevathan, 'Cortisol reactivity, maternal sensitivity, and learning in 3-month-old infants' (2008) Infant Behaviour & Development Vol 92, p106.
Verdecias et al, 'Attachment styles and sleep measures in a community-based sample of older adults' (2009) 10 Sleep Medicine 664.
Wüst et al, 'Habituation of cortisol responses to repeated psychosocial stress-further characterization and impact of genetic factors' (2005) Psychoneuroendocrinology Vol 30, p199.










Wow, what a thought provoking article.
ReplyDeleteMakes me grateful I have chosen to bring up my kids with attached parenting.
Thanks
Carly Ballard
amazing!! We AP parent too, thank god!
ReplyDeleteHi I have been thinking about this as recently there seems to be alot of research and blogs on the subject. Although HP don't advise controlled crying, they do say (in the UK) that is it only ok after the baby is 6 months. How can that be though when, for the 1st year, the mothers body should be the infants environment. I would think that if your child requests (in any way) your physical presence and affection you should be there for them, whether they are 2 months, 2 years or 2 decades old! But what about tantrums? For example when DD1 was 15 months old she would wake the odd night and use a bottle of warm milk (cows) to get back to sleep. Bottles are not recommended after the age of 1yr and she did not need the milk nutritionally so we decided to stop offering it. (had she been still BFing I would not have declined her that!) She of course threw a tantrum. We dealt with this as we do most tantrums. Ignore the behaviour but not the child. So I kept going in and cuddling her and placing her back in bed and offering her a drink of water until she went back to sleep. Its just this felt a bit like controlled crying and I'm worried now that I didn't handle it as well as I could. I'm trying to AP the best I can but its tricky when confronted with a screaming toddler! What are your thoughts?
ReplyDeleteHi Rosie,
ReplyDeleteI'm no expert on these things. They are difficult questions, and I'm not sure there even is a 'right answer'. I have pushed my daughter down to 2 feeds a night when she was feeding on demand 7-8 times. I did this at 10mo by cuddling and offering water, and initially she was v unhappy about it. But I have my limits.
I don't think there's any scientific or community consensus on the effect this has on the child. I think it also depends on the child. I think your approach sounds very loving and sensitive, and I think a 15mo in a loving family would usually have the capacity to learn to wait till morning for a feed. And even if they find the process distressing, I would think you could move past that by taking time to connect with each other in other ways.
I believe there are tooth decay issues with falling asleep on the bottle, as the milk pools in their mouth and the sugars sit on their teeth.
Just personally, I wouldn't think of a strong negative reaction at that age as a tantrum so much as a genuine protest. But I don't think that means it's damaging to say no, particularly when you are present and loving in the way you say it. Have you read my review of the Alicia Lieberman book? It has some stuff about tantrums.
I suppose it's good to reflect on what we do as parents, but kids also respond to calm, self-confidence, so don't forget to also be proud of the effort you put into parenting. Set realistic expectations, and if you make a mistake, learn from it and forgive yourself.
You sound like a very dedicated, caring mum to me!
Thank you. I will ck out the review. She seems fairly well balanced and adapted to having a sister pretty well so must have done something right!! Who knew child rearing was such a minefield of conflicting advice!? Thanks again, Rosie xx
ReplyDeleteAs a grandmother I am so exited this this information is eventually coming out! Of course a small baby (up to about a year) has only 3 demands - Mommy milk(or substitute), Mommy's arms and please change diaper! I discovered "attachment parenting" with my 3rd child, what a difference it made to his character (compared to the previous 2) He seldom cried, and has grown inot a senstive young man, who is about to become a Father , the benefits also rubbed off onto my daughter, who has become an attachment parent herself! Viva A.P !!
ReplyDeleteTHANK YOU, THANK YOU, THANK YOU!!! as someone who has been advocating for years the ill effects of crying methods, i can't thank you enough for putting together such concise and good information. i have been trying to work on a similar project and it is quite daunting... but, you have don't it so well. THANK YOU!
ReplyDeleteThank you for putting together such a detailed series on this topic. As a new mum I am constantly feeling guilty and confused as to whether I am doing the right thing when it comes to sleep for my son, myself and our sanity. My boy is a terrible sleeper most nights (on a bad night it's waking every hour) and will surprise us every now and then with nights of longer 4-5 hour blocks. I am not comfortable with CIO and know I would be pretty hopeless with controlled crying. So it's good to know that I am not 'spoiling' him or creating bad habits by comforting/cuddling bringing him into bed with us. Of note he goes to sleep on his own for 80% of his naps and will self settle from one cycle to another during the day, he just does not like bedtime. I am surrounded by AP mums and it's good to know there is evidence out there supporting this approach because when you hear about other babies sleeping through the night, the self doubt creeps in. Thanks so much for putting this together.
ReplyDelete